Precision Medicine Sends Cancer for a Loop
In a tour de force of precision medicine, an international team led by two Columbia University Herbert Irving Comprehensive Cancer Center (HICCC) researchers has demonstrated the potential of a new approach to prostate cancer treatment. The iterative strategy, named OncoLoop, uses a sophisticated computer algorithm to match each patient to an “avatar” -- a carefully engineered laboratory model of a cancer that matches the molecular profile of the patient's tumor. By selecting drugs that target the master regulator proteins responsible for the genetic program driving the avatar’s tumor, the team can then validate the treatment regimen most likely to work in that patient.
“We take a patient, we match them to the set of mouse tumors we already have, and to the set of drug data that we already have, and then actually identify drugs that are most likely to work in both the patient and the model … test those drugs in those models, and then use that information to inform clinical treatment,” says Cory Abate-Shen, PhD, a senior author on the new work and member of the HICCC and department chair of Molecular Pharmacology and Therapeutics at Columbia University Vagelos College of Physicians and Surgeons (VP&S).
The strategy solves a fundamental problem in cancer drug research: cellular and animal models of the disease are often considered to be poor mimics of any particular patient’s tumor. “There’s been tremendous controversy around what is a good model, and so we decided that maybe we needed a more quantitative and sophisticated approach,” says Andrea Califano, Dr., chair of the Department of Systems Biology at VP&S and co-leader of the Precision Oncology and Systems Biology program at the HICCC. Dr. Califano is also a senior author on the new paper, published in Cancer Discovery.
To accomplish that, Drs. Abate-Shen, Califano, and their collaborators at Columbia University Irving Medical Center and several other research institutes combined algorithmic mining of large sets of patient data with a collection of genetically engineered mice that replicate different types of genetic dysregulation found in prostate cancers, providing researchers with dozens of models of prostate cancer that can more closely mimic the heterogeneous tumor types found in patients. Until recently, though, that would’ve seemed like an impossible task.
“If you look at the number of genes whose mutations are potentially associated with cancer, there are about 2,000 of them; if you look at all the possible ways in which you could combine them, you get more potentially tumorigenic patterns than there are atoms in the universe,” says Dr. Califano. However, the researchers have shown that the majority of such tumorigenic patterns are processed by a limited set of master regulator proteins.
“Think of cancer mutations as grains of sand in the upper part of an hourglass,” says Dr. Califano, adding that “you don’t need to shoot every single grain of sand, because, if you just block the middle point they all have to go through to reach the bottom, the hourglass will stop working.”
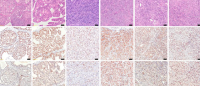
In the OncoLoop approach, the investigators analyze the gene regulation profile of a patient’s cancer to determine which master regulators are involved, and select an avatar model with the same master regulator profile. They can then identify drugs likely to invert the activities of those master regulators to kill the tumor cells instead of preserving them, and test those drugs individually or in combination on the patient’s avatar model to validate them.
Besides providing treatment plans that attack the patient’s tumor most effectively, the strategy also makes it less likely that the cancer will evolve resistance to the regimen. “By getting drugs that invert the master regulator program, you’re not hitting on one particular target, [but] the focal point, and it becomes very, very hard for the cell to get around that,” says Dr. Abate-Shen. The limited number of master regulators also means that once the team has identified an effective treatment for a given profile, it should work in other patients who share the same profile.
While prostate cancer provided an ideal system in which to prove that the concept works, OncoLoop could see broader use. “We are already running a number of clinical trials where we’re using these [methods] in other tumors,” says Dr. Califano.
Both researchers emphasize that cross-disciplinary collaboration was crucial to the project's success. "Our models are great models, but they wouldn't be as valuable as they are without the algorithms, and the algorithms are really valuable because they're applied to biologically relevant models," says Dr. Abate-Shen. Dr. Califano adds that "that's why we've been working together for the last twelve years."
References
Vasciaveo A, Arriaga JM, Nunes de Almeida F, Zou M, Douglass EF, Picech F, Shibata M, Rodriguez-Calero A, de Brot S, Mitrofanova A, Chua CW, Karan C, Realubit R, Pampou S, Kim JY, Afari SN, Mukhammadov T, Zanella L, Corey E, Alvarez MJ, Rubin MA, Shen MM, Califano A, Abate-Shen C. OncoLoop: A network-based precision cancer medicine framework. Cancer Discov. 2022 Nov 14


