Pancreatic Cancer
Make an Appointment
Our team of dedicated access representatives is here to help you make an appointment with the specialists that you need.
Your pancreas is a fish-shaped organ in your upper abdomen between your stomach and intestines. It’s composed of two lobes that work together to help you digest food and produce hormones, including insulin and glucagon, to keep your blood sugar in balance.
Types of Pancreatic Cancer
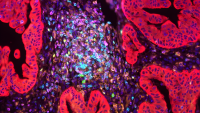
When cells inside your pancreas grow abnormally, it’s called pancreatic cancer. Cells clump into masses called tumors. There are several types of pancreatic cancer. Each type is diagnosed and treated differently. It is critical to have a skilled and experienced pathologist determine what type of pancreatic cancer you have.
Exocrine Tumors
More than 90% of pancreatic tumors are called ductal adenocarcinomas; this is the disease that people think of as pancreatic cancer. Most tumors are found in the pancreas head, closest to the duodenum and bile ducts. These tumors may spread to nearby organs, including your bile ducts, intestines, and stomach. They may also spread to adjacent blood vessels, lymph nodes, or into your bloodstream, where they deposit into your liver and other organs. Since tumors in the pancreas head often block bile ducts, many people show signs of jaundice—yellowing of your skin and eyes. Jaundice can help doctors diagnose pancreatic cancer before it spreads.
Ampullary cancer, a rare form of pancreatic cancer, starts where the bile duct coming from your liver and the pancreatic duct meet and drain into your small intestine. These tumors are generally less aggressive. They are technically not considered pancreatic cancer, but they are often treated similarly.
Endocrine Tumors
Five to 10% of pancreatic cancer are endocrine tumors. They’re also called islet cell tumors and pancreatic neuroendocrine tumors (PNETS).
These tumors are treated differently than pancreatic adenocarcinomas. They’re sensitive to drugs that block blood vessel formation and to different types of chemotherapy. They usually have a better prognosis than adenocarcinomas.
Risk Factors
Pancreatic cancer makes up just 2.8% of new cancer diagnoses in the US, according to the American Cancer Society. About 46,000 people will be diagnosed here. The numbers in the US and Europe are growing relative to the rate of other types of cancer. Pancreatic cancer is the fourth leading cause of cancer in the US.
Because symptoms of pancreatic cancer are rather general, most people are not diagnosed until after it has spread and is hard to cure. Risk factors include:
- Age. Most people are diagnosed with pancreatic cancer between the ages of 60 and 80.
- Race and ethnicity. African Americans have a higher rate of pancreatic cancer, as do people of Ashkenazi Jewish descent.
- Smoking. People who smoke cigarettes are about twice as likely to develop pancreatic cancer as those who don’t. And smoking-related tumors tend to grow faster and develop about 10 years earlier than other tumors. About 20% of pancreatic cancer is associated with smoking.
- Diabetes. People who have diabetes are twice as likely to develop pancreatic cancer as those without the disease. However, doctors don’t fully understand the relationship between the two diseases. Glucose intolerance, a sign of diabetes, sometimes is caused by changes cancer makes to the pancreas.
- Pancreatitis. This acute or chronic inflammation of the pancreas increases your risk of pancreatic cancer. Chronic pancreatitis is typically diagnosed between ages 35 and 45. Genetic factors, malformed pancreas ducts, trauma, and heavy alcohol use can cause this disease. Some people have inherited genetic mutations that lead to pancreatitis at an early age. These genes also increase the risk for pancreatic cancer.
- Family history. If your mother, father, sibling, or child has had pancreatic cancer, your risk increases by two to three times—more if multiple people have had it. Doctors have linked several inherited gene mutations with this increased risk, including the genes responsible for breast cancer, ovarian cancer, and melanoma.
- Diet. Eating a lot of red meat and fat is associated with pancreatic cancer.
- Obesity. A BMI above 25 can increase the risk of developing pancreatic cancer.
- Chemical exposure. Exposure at work or elsewhere to pesticides, dyes, or gasoline-related chemicals can increase pancreatic cancer risk.
- Pancreatic cysts. Some types of cysts inside your pancreas can progress to cancer. We have a screening program dedicated to people with these cysts.
Signs of Pancreatic Cancer
Pancreatic cancer can have symptoms similar to viral hepatitis or gallstones, or no symptoms at all. Because of this, it’s often diagnosed after it has spread. Symptoms may include:
- Pain in the upper abdomen, often with pain in the back directly behind the upper abdomen
- Unexplained weight loss
- Jaundice
- Itchy skin
- Nausea
- Loss of appetite
- Diarrhea
- Fatigue
- Floating or foul-smelling stools
- Depression
- Ascites, a condition in which excessive fluid builds up in the abdominal cavity causing swelling and distention of the belly and, sometimes, pain and difficulty breathing
- New or sudden worsening of diabetes
- Dark stools
- Difficulty swallowing, which becomes worse over time
- Excessive burping
- General decline in health
- Loss of appetite or feeling full early after starting to eat
- Nausea
- Vomiting blood
- Weakness or fatigue
Screening and Diagnosis
Symptoms of pancreatic cancer aren’t always obvious. The disease can also develop gradually and be mistaken for other conditions. Sometimes tumors are found accidentally when you’re being evaluated for another medical condition. If your doctor suspects pancreatic cancer, you may have many or all of these tests.
Physical Exam
Your doctor will take your medical history and pinpoint risk factors and family histories. They’ll check your abdomen for masses or fluid buildup and check your skin and eyes for signs of jaundice. They may also examine the lymph nodes above your collarbone and in other parts of your body in case cancer has spread. They may also order urine and stool tests.
Blood Tests
There is no simple blood test for pancreatic cancer. But other blood tests can help hone in on the diagnosis.
- Hepatic function. This test measures bilirubin and liver enzyme levels in the blood.
- CA 19-9 tumor marker. CA 19-9 is a substance a tumor or your body releases into your bloodstream in response to tumor cells. This marker is commonly—but not always—elevated in pancreatic cancer.
- Carcinoembrionic antigen (CEA). CEA is a protein that may also be a tumor marker. The CEA test can determine how far the disease has progressed and how effective treatment is.
Imaging Tests
These noninvasive tests can show a mass in your pancreas and help determine if you are a suitable candidate for surgery.
- Abdominal ultrasound uses sound waves to show images of your internal organs.
- CT (computed tomography) scan takes data from several X-ray images of the body and converts them into pictures on a monitor. It can show tissues and blood vessels in addition to bones.
- MRI (magnetic resonance imaging) test uses powerful magnetic fields to create 3D pictures that detect tumors in your pancreas.
- MRCP (magnetic resonance cholangiopancreatography) helps your doctor noninvasively visualize the bile and pancreatic ducts, which is particularly helpful since tumors typically start in the ducts.
- PET (positron emission tomography) scan uses a small amount of radioactive glucose injected into your vein to show where glucose is being used in your body. A scanner rotates around your body to create an overall picture. Cancer cells use more glucose than normal cells do.
Other Tests
If your doctor suspects pancreatic cancer, they may order these tests:
- SpyGlass direct viualization system. We are the among the first in the nation to use this innovative new technology to visualize and evaluate hard-to-access pancreatic ducts with greater clarity.
- Endoscopic transesophageal ultrasound (EUS), usually an outpatient test, uses sound waves to visualize tumor depth, surrounding lymph nodes, and the tumor's relationship to adjacent structures. It uses a thin lighted tube called an endoscope with an ultrasound probe on the tip. Your doctor can take a biopsy of a suspicious cyst or suspected tumor.
- Endoscopic retrograde cholangiopancreatography (ERCP) allows your doctor to visualize the bile and pancreatic ducts using an endoscope, dye injected directly into your pancreas and bit ducts, and an X-ray. It’s usually done if you have signs of jaundice, which can indicate a blocked bile duct.
- Biopsies, or a tissue sample of the suspected cancer, can be done three ways:
- Fine needle aspiration or core biopsy directly samples the suspicious lesion through your skin or guided by an endoscopic transesophageal ultrasound. If done through your skin with a local anesthetic, they’ll use a CT or ultrasound to guide the needle placement.
- Brush biopsy uses a small brush inserted directly into the bile or pancreatic duct through an endoscope during an ERCP. Cells rub off on the brush, then a pathologist examines the cells under a microscope for changes indicating cancer.
- Laparoscopy uses a small incision to pass a thin tube with a light and video camera to directly view the pancreas and surrounding organs while you’re under general anesthesia. They can take a tissue biopsy during this procedure.
These tests can also help doctors visualize the cancer’s spread and determine if it can be removed, called staging.
Staging
When your doctor estimates your prognosis based on how much cancer is in your body and where it is, that’s called staging.
- Stage 0. Carcinoma in situ. In this early stage of cancer, abnormal cells grow in your pancreas’s ducts or lining but have not spread outside of the organ.
- Stage I. Cancer is confined to your pancreas. A stage IA tumor is 2 cm or smaller. A stage IB tumor is larger than 2 cm.
- Stage II. Cancer has spread to nearby lymph nodes but doesn’t involve local blood vessels or distant parts of your body.
- Stage III. Cancer has spread to nearby blood vessels, but has not invaded distant organs or tissue. Cancer may or may not be in local lymph nodes.
- Stage IV. Cancer has spread outside the pancreas to other parts of your body.