Bone Marrow/Stem Cell Transplantation
Patients across the nation, and worldwide, come to the Herbert Irving Comprehensive Cancer Center at New York-Presbyterian/Columbia University Medical Center for truly individualized care.
Recognized by the National Cancer Institute as a designated comprehensive cancer center, our program provides access to specialists in every discipline, offering the kind of in-depth expertise only possible at a major academic medical institution.
Our physicians are global leaders in innovative technologies, genetics, clinical trials and "bench to bedside" research, allowing us to offer the most advanced therapies for diseases requiring bone marrow or stem cell transplants.
Approach and Expertise
The Blood and Marrow Transplantation Program at New York-Presbyterian/Columbia University Irving Medical Center (NYP/CUIMC) offers a multidisciplinary approach to patients undergoing a stem cell or bone marrow transplant. Our team consists of nationally and internationally known experts in the field of hematology, oncology and radiation therapy. Together with highly experienced and specialized nurses and nurse practitioners we provide comprehensive care for all of our patients.
In addition to providing state of the art treatment for patient undergoing autologous or allogeneic stem cell transplantation our BMT program is at the forefront of studying new approaches to making transplant safer and more effective by reducing transplant related complication and the relapse rates after transplant. In particular our program is focusing on developing novel therapeutic strategies to prevent and treat Graft versus Host Disease one of the most common and serious side effects of allogeneic BMT.
Apart from developing novel approaches to preventing GVHD our program is conducting research to on cellular therapy approaches to prevent recurrence after allogeneic transplant.
Bone Marrow Transplantation has a huge potential and cannot only be used to cure blood cancers or benign bone marrow disorders, but can also be used to treat autoimmune disorders. Furthermore, BMT has been shown to induce true immunological tolerance meaning full graft acceptance without the need for lifelong immunosuppression. To this end the BMT program is working closely together with the Columbia Center for Translational Immunology to develop treatment protocols to avoid the use of life-long immunosuppression in the setting of solid organ transplantation by combining BMT and solid organ transplantation.
About Bone Marrow/Stem Cell Transplantation
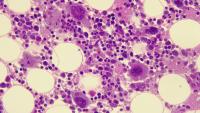
Bone marrow is found in the spaces in the center of your long bones in your body. Blood cells are made in the bone marrow: white blood cells (WBC) fight infection; red blood cells (RBC) carry oxygen; and platelets (PLT) help form clots to prevent bleeding. Stem cells are blood cells that have not yet become a specific kind of blood cell. All cells begin as stem cells. By transplanting stem cells we can regenerate your blood cell forming ability. Stem cells tend to remain in the bone marrow, where they can become any type of blood cell the body needs, but some go into general circulation in the blood vessels.
Bone Marrow or Stem Cell Transplant
A bone marrow transplant can also be referred to as a stem cell transplant and is a method of treating patients with specific types of cancers or bone marrow diseases. Examples of cancers and diseases that are treated with a stem cell transplant include leukemia, lymphoma, and multiple myeloma, amyloidosis and various inherited blood diseases like sickle cell anemia.
The decision to transplant and the type of transplant that a patient receives depend on a number of factors. These factors include the type and stage of cancer or disease, the availability of a suitable donor, and the potential risks and benefits for the patient.
There are two basic types of stem cell transplants. The types of transplants are named according to who donated the stem cells. If the person donating the stem cells is the patient, the transplant is called an autologous transplant or Auto for short (Auto means self). If the stem cells are donated by someone other than the patient, the transplant is called an allogeneic transplant or Allo for short (Allo means other). The person donating stem cells for an allo transplant can be a relative of the patient or someone not related to the patient. Before either type of transplant, a patient will receive high-dose chemotherapy, or a combination of chemotherapy and radiation. This prepares the body for the transplant by eliminating any abnormal or cancer cells in the patient’s blood stream and by destroying blood-forming cells in the marrow, to make room for new cells.
Autologous Stem Cell Transplant
Autologous means “from yourself.” Stem cells will form your new bone marrow after you have been treated. The stem cells in your blood are collected (harvested) before you are treated with high-dose chemotherapy called the “conditioning regimen.” We call this stem cell harvesting. You will have injections of G-CSF (Neupogen©) to help your body make more stem cells.
Stem cell harvesting is done in the Blood Donor Room and is very similar to giving blood. You will sit in a chair or lie in a bed. You can read or listen to music throughout your time there. It takes between three to four hours for each collection day. Several harvesting procedures (1 – 5) may be required to get enough stem cells to support an autologous stem cell transplant. With an Autologous Transplant, we know that your type of cancer responds to high doses of chemotherapy, radiation or both. A side effect of these is that your bone marrow will be wiped out. When your treatments are finished, the stem cells will be given back to you (“transplanted”) Diseases that we treat with Autologous Stem Cell Transplant include Lymphoma, Multiple Myeloma, Amyloidosis.
Allogeneic Stem Cell Transplant
An allogeneic stem cell transplant replaces your stem cells with new, healthy ones from a donor. “Allogeneic” means that the stem cells come from a donor other than you. You will have chemotherapy, radiation, or both to treat your cancer and/or suppress your immune system. This will damage your normal bone marrow. You will then receive the transplant of the donor stem cells.
Allogeneic transplants are used to treat many diseases. These include Leukemia, Lymphoma, Aplastic Anemia, Sickle Cell Anemia or other tumors and immune deficiencies that are present form birth. The care you need before a transplant depends on your disease. Your doctor will tell you why a transplant is used, why you cannot use your own stem cells, and what treatment plan is best for you.
Your Doctor will decide which type of donor is best for you. It can be a related or unrelated donor. The right donor is someone whose tissue type most closely matches yours. Family members will have a blood test to see what tissue type they have. If no family member is a close match, your doctor will start a search with a donor registry. Depending on the situation a half-matched or haploidentical family donor may be utilized if a fully matched unrelated donor cannot be identified.
Myeloablative Transplant versus Non-Myeloablative Transplant
There are two approaches to treatment before an allogeneic transplant. One is called myeloablative. With this approach you receive high doses of chemotherapy with or without radiation. These treatments aim to kill your cancer but also kill (myeloablate) all stem cells in your bone marrow. The donor stem cells will then replace the ones killed by the treatment. This form of treatment is very strong and it may not be suitable for all patients.
Another approach involves a less intense treatment. It uses lower doses of chemotherapy with or without low doses of radiation. It also includes drugs that suppress your immune system. This type of transplant is called non-myeloablative or reduced-intensity conditioning. It aims to weaken your immune system and destroy enough stem cells to allow the donor stem cells to take over.
Your doctor will consider many factors when choosing which type of transplant is best for you. These include your disease, other treatments you have received, and your general health status.
How is a Bone Marrow/Stem Cell Transplant Done?
The transplant itself is not considered a surgery. Stem cells are infused into the patient's bloodstream intravenously much in the same way a blood transfusion is given.
It takes about a week for the new stem cells to find their way to the bone marrow. Once there, they begin to manufacture healthy cells, including red and white blood cells and platelets.
After several weeks, the body’s blood supply is replenished, and if the transplant is a success, the patient’s bone marrow is restored and begins making mature blood cells. Until that happens, however, the individual must be protected from infections and any activity or injury that might cause bleeding. As a result, Autologous transplant patients are usually hospitalized and carefully monitored for 2-3 weeks and Allogeneic transplants about 4 weeks. You will also be monitored very closely once you are discharged from the hospital.
Who is Eligible for a Bone Marrow or Stem Cell Transplant?
• In the early stages of disease
• In remission or there is very little disease in the body
• Responsive to chemotherapy
• In good general health
Caregiver Responsibilities
The role of the caregiver in the transplant process is extremely important. Often the success of the transplant depends, in part, on the interactions between the patient, the caregiver, and the transplant team.
As a caregiver, you will receive specific instructions from the transplant doctors and nurses on the best ways to help the patient. Remember that you are part of the transplant team and that the other members of the team are ready to assist you in every possible way to make sure that the transplant process proceeds well.
If you have questions, please feel free to ask so that you feel comfortable in your role and understand the care requirements. Together, we can provide excellent care for the patient and achieve a successful outcome.
Diseases We Treat
We offer the full array of blood and marrow transplantation services including autologous, allogeneic, myeloablative and reduced intensity transplant depending on the type and stage of disease.
In addition to offering transplants to patients with acute and chronic leukemias, myeloproliferative and myelodysplastic disorders, we have a particular focus on patients with:
- Lymphomas (Non-Hodgkin/Hodgkin Lymphoma)
- Plasmacell dyscrasias (Amyloidosis and Multiple Myeloma)
- Sickle Cell Disease
The BMT program at Columbia University Medical Center is closely integrated with the primary referring disease centers at Columbia (i.e. Amyloidosis and Myeloma Service, Center for Lymphoid Malignancies, MDS Center, Leukemia Service) and works closely with the referring oncologists outside of Columbia in order to provide the most cohesive and integrated continuity of care for our transplant patients.
Bone Marrow Transplant Service
The Foundation for the Accreditation of Cellular Therapy (FACT)-accredited Bone Marrow Transplant Service at CUIMC is comprised of many people:
- Your own doctor, the one that you see when you are an outpatient, will be in charge of your care throughout your treatment.
- Nurse practitioners and physician assistants are also partners in your care.
- A nurse practitioner is a nurse who has an advanced degree in an area of care. This nurse practitioner can take patient histories, do physical exams, and prescribe treatments and medicine. He or she can also provide medical care with the doctors.
- A physician assistant also had advanced medical training and can do the same tasks as a nurse practitioner can do, however he or she has not had nursing training.
- A team of primary nurses will be responsible for your day-to-day nursing care while you are in the hospital. You will also be in contact with nursing attendants, a pharmacist who specializes in stem cell transplant, nutritionist and dietary aids and social workers.
- Since we are a teaching hospital and associated with Columbia University, you will also meet interns and residents who are working with the team throughout your stay.
The transplant team also includes physicians from other specialties who may need to be involved in your care like nephrologists, cardiologists or dermatologists. Furthermore, our team is complemented by a psychiatrist who provides psychological support to patients undergoing autologous or allogeneic transplant.
Additional Resources
- Association of Cancer Online Resources (212) 226-5525
- Be the Match (888) 999-6743
- Bone Marrow Foundation (800) 365-1336
- BMT Infonet (888) 597-7674
- Cancer Care Inc. (800) 813-4675
- Cutaneous Lymphoma Foundation (248) 644-9014
- Fertile Hope (888) 994-4673
- Hope Lodge (800) 227-2345
- International Myeloma Foundation (800) 452-2873
- Leukemia and Lymphoma Society (212) 448-9206
- Leukemia Research Foundation (888) 558-5385
- Lymphoma Research Foundation (212) 349-2910