Myelodysplastic Syndrome
Make an Appointment
Our team of dedicated access representatives is here to help you make an appointment with the specialists that you need.
Myelodysplastic syndromes (MDS) are a group of diseases affecting the blood and bone marrow—the soft, spongy area at the center of bones. The American Cancer Society estimates that 12,000 to 15,000 people in the US will be diagnosed with a myelodysplastic syndrome this year. This is considered a rare disease.
Bone marrow works like a factory. It produces stem cells that can create many other cells. This critical function is called hematopoiesis. Stem cells turn into red blood cells that carry oxygen, platelets that prevent bleeding, and white blood cells that fight infection.
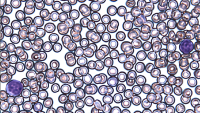
In MDS, stem cells make too many blood cells. Some die prematurely and never make it out of the marrow. Others don’t mature properly. As a result, the entire blood production process gets interrupted and thrown off track.
Causes of MDS
Primary, or de novo, MDS has no known cause. Most people fall into this category. Prior chemotherapy or radiation therapy for a previous cancer causes secondary MDS.
Risk Factors
If you’re diagnosed with a myelodysplastic syndrome, it’s not your fault. Risk factors for myelodysplastic syndromes are mostly out of your control. They include:
- Age. Most people with MDS are over 60. Although you can develop it at any time of life, it’s rarely diagnosed in people under 40. The incidence of MDS is rising as the population ages.
- Previous cancer treatment. People who’ve had both chemotherapy and radiation for another cancer have the highest risk of MDS, though their overall risk is still considered low.
- Gender. MDS is more common in men than women.
- Smoking. Use of cigarettes is a known risk factor.
- Environmental causes. Exposure to high levels of radiation, to benzene, and to some chemicals used in the petroleum and rubber industries have been linked to MDS.
- Inherited syndromes. Fanconi anemia, Shwachman-Diamond syndrome, familial platelet disorder, and severe congenital neutropenia are associated with MDS.
Symptoms
People are often diagnosed with MDS when their doctor finds abnormal blood counts during a routine physical exam. The symptoms depend on the type of blood cell that’s being affected.
- Low red blood cells lead to anemia: Headaches, lightheadedness, shortness of breath, pallor, and fatigue
- Low white blood cells cause an increased risk of infections that are recurrent and difficult to treat
- Low platelets cause bruising, frequent nosebleeds, and red spots (petichiae) on the skin
Diagnosis
A hematologist/oncologist who specializes in blood disorders diagnoses myelodysplastic syndromes using some or all of the following tests.
A complete blood count (CBC) gives your doctor a profile of your blood. It shows whether your bone marrow is making fewer white cells, red cells, platelets, or all three. If you’re anemic, additional tests can help determine if it’s caused by MDS or iron, vitamin B12, or folate deficiencies.
Bone marrow aspiration or biopsy uses a needle to sample marrow fluid (aspiration) and/or solid bone marrow tissue (core biopsy). This sampling usually happens at the back of your hip after numbing the area. A pathologist will then examine the cells under a microscope for abnormalities and to rule out other types of cancer.
Classification
MDS is divided into a spectrum from very low risk to very high risk, according to the American Cancer Society. The risk is whether the syndrome will progress to acute myeloid leukemia.
Lower-risk MDS results in fewer red blood cells, called anemia, but few other issues.
High-risk MDS is sometimes called pre-leukemia or smoldering leukemia. In this case, the number of immature white blood cells in bone marrow—called blasts or dysplastic cells—can increase, crowding out healthy cells. It progresses to acute myeloid leukemia in about 30% of people.
The World Health Organization describes eight kinds of MDS. They are based on changes in your blood-making process. These categories reflect the number of myeloblasts, abnormal red blood cell precursors, called ringed sideroblasts, and abnormal dysplastic cell types, in the bone marrow. They also reflect your bone marrow cells’ genetic profile.
- MDS with single lineage dysplasia (MDS-SLD)
- MDS with multilineage dysplasis (MDS-MLD)
- MDS with ring sideroblasts and single lineage dysplasia (MDS-RS-SLD)
- MDS with ring sideroblasts and multilineage dysplasia (MDS-RS-MLD)
- MDS with isolated deletion of chromosome 5q
- MDS with excess blasts-1 (MDS-EB-1)
- MDS with excess blasts-2 (MDS-EB-2)
- MDS-unclassifiable (MDS-U)
With rare exceptions, people with MDS-SLD, MDS-MLD, MDS-RS-SLD, MDS-RS-MLD, and MDS with deletion of chromosome 5 belong to the lower risk category.
Staging
Doctors generally use the revised International Prognostic Scoring System (IPSS-R) to determine your prognosis and risk for developing acute leukemia. It also helps them know when to start treatment and choose the most appropriate treatment. IPSS takes into account:
- The percentage of blasts (immature blood cells) in the bone marrow
- Complete blood count results
- Certain genetic abnormalities
Your score is calculated after you have a blood test and bone marrow biopsy.